- Subject Code : 401211
- University : Western Sydney University My Assignment Services is not sponsored or endorsed by this college or university.
- Subject Name : Health Variations
Case study questions
Solution 1: Pathogenesis of Asthma
Asthma is a chronic condition associated with the inflammation of the airways. This inflammation could be triggered by an allergen cascading an immunogenic response involving the neutrophils, eosinophils, mast cells, lymphocytes and the epithelial cells in the respiratory tract (Carpaijj et al., 2019). The airway flow in the respiratory tract is constricted in asthma leading to shortness of breath in the patient. This constriction in acute exacerbated asthma is a direct consequence of bronchoconstriction, which is smooth muscle contraction narrowing the airway passage. At a molecular level, the concentration of immunoglobulin E is increased in the pathway triggering the reaction of the immune system of the body. This results in hyperresponsiveness of the body and leading to airway inflammation. This inflammation works as a direct hindrance to the airflow causing breathing difficulties and causing asthma in Poppy (Boulet, 2017).
In patients, asthma can be defined based on intermittent or persistent symptoms and the severity. The body response to asthma incorporates a reaction from the adaptive immune system, respiratory epithelium and the innate immune system. The epithelial injury and inflammation in the respiratory tract include eosinophils, lymphocytes, phagocytes and mast cells. These cells release the inflammation mediators that are inclusive of the cytokines, lymphokines and chemokines. These further triggers the immunogenic response and induce a bronchospasm that leads to damaging the epithelium. A cycle of inflammation is thus created producing a chronic condition in the patient. When asthma is triggered by an allergen the Antigen presenting cells of the body play role in triggering of the inflammatory response (Carpaijj et al., 2019).The airway epithelium is responsible for the release of several kinds of inflammatory molecules that include TNF-α, IL-1β, and IL-6 that upregulate the inflammatory genes and stimulates the T cells. The T cell stimulation activates the effector leukocytes to the airway and further causes chronic inflammation in the patients. Mast cells serve as the key regulators of the inflammatory reaction pathway and lead to airway obstruction in the patients and lead to difficulty in breathing in the patients. The chemokines released in the airway pathway are crucial for the movement of the inflammatory cells to the airway pathway (Boulet, 2017). The inflammatory response results to modeling of the bronchial tissue along with the activation of the epithelial-mesenchymal trophic unit. This damage alters the point of contact between the epithelial cells and the mesenchymal trophic unit, inducing the structural changes throughout the respiratory tract (Boulet, 2017).
These compounds direct the movement of the cells towards the airway and further result in obstructing the air pathway leading to shortness of breath in Poppy and cause a respiratory distress.
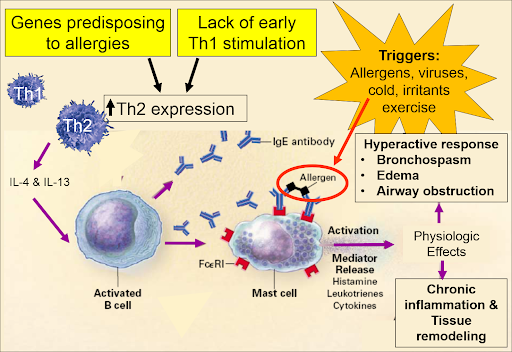
Figure 1: Pathogenesis of asthma (Boulet, 2017)
Solution 2:
Part A: High Fowlers positioning in respiratory distress.
The high fowler's position angles the patient to 30degrees to 90degrees. This facilitates the relaxation of tension built in the abdominal muscles and thus aids in breathing. The position releases the compression pressure on the chest that occurs due to gravity and assists Poppy in breathing (Sousa &Warren, 2017).
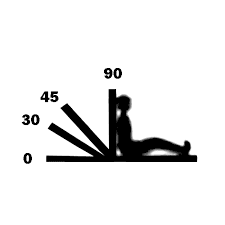
Figure 2: High Fowler positioning (Sousa &Warren, 2017)
Part B: i) Suitable oxygen device: Hudson mask
ii) Rationale for selection:Hudson mask is an efficient means to provide high flow oxygen therapy to manage asthma. The device is used to provide supplemented oxygen to a patient with breathing difficulties like asthma. The device is a composite of a breathing mask placed on the nostrils of the patient through which supplemented airflow is provided. A Hudson mask is suited for children like Poppy as it aids in ease of respiratory distress without causing much discomfort. (Wilkinson et al., 2018).
iii) Mode of function of supplemented oxygen: supplemented oxygen reduces the negative drain created by reduced oxygen saturation and provides the lungs with extra oxygen by opening up the airways (Boulet, 2017).
Solution 3:
Part A: Salbutamol via nebulizer
i) Mechanism of action: Salbutamol acts as an antagonist to the selective beta2-adrenoceptor. The drug acts on the receptors of the bronchial muscles and dilates them. This phenomenon is known as bronchodilation. The mechanism of action of this drug is fast as it acts within five minutes of administration (Zhou et al., 2017).
ii)Rationale for medication: The administration of salbutamol via nebulizer will cause bronchodilation and improve the respiration in the patient by easing the breathing cycle.
iii)Nursing considerations of medication: The nurse needs to check the heart rate and blood pressure of the patient before and after administration of the drug. It is also prohibited in patients who are hypertensive and have cardiac problems that may be elevated by this drug (Zhou et al., 2017).
iv) Expected clinical response: The expected clinical responses include normalization of oxygen saturation levels, normalization of respiratory rates and ease in breathing in a patient. Restoration of blood pressure to normal (Zhao et al., 2020).
v) Continuing clinical observations required: The clinical assessments include analysis of lung sounds, evaluation of vitals, blood pressure and heart rate evaluation before and after administration of the medication. In case of presence of cough, the nature of cough and sputum must be analyzed (Zhao et al., 2020).
Part B: Hydrocortisone IV
i) Mechanism of action: The medication is used in asthma as it enhances the beta-adrenergic response and eases the muscle spasm in the patient. The drug also functions by reversing the mucosal edema that may be a cause of airway hindrance. The drug decreases the vascular permeability through vasoconstriction and inhibits the release of LTD4 and LTC4 aiding an asthmatic patient in breathing (Adlan et al., 2018).
ii)Rationale for medication: The drug clears out the airways and allows the patient to breathe more easily this aidin providing relief to the patientthrough an anti-inflammatory effect on the body (Barabutis et al., 2017)
iii)Nursing considerations of medication: The drug administration causes an elevation in blood pressure. Therefore, the blood pressure and the heart rate of the patient before and after drug administration must be critically monitored. It may also cause side effects like headaches, fluid retention and puffiness on the face (Adlan et al., 2018).
iv) Expected clinical response: The expected clinical response will be normalization of the vitals. That is the restoration of the blood pressure and heart rate of the patient alongwith regularization of the oxygen saturation levels in the patient and overall improvement in the breathing cycle (Barabutis et al., 2017).
v) Continuing clinical observations required: Monitoring of vitals and analyzing the response to the medication is critical (Adlan et al., 2018).
Part C: Ipratropium Bromide via nebulizer
i)Mechanism of action: Ipratropium Bromide is a parasympatholytic agent that is an anticholinergic agent and functions by blocking the muscarinic receptors of acetylcholine. The medication functions as a bronchodilator and enlarged the airway for smooth passage of air for the ease of breathing (Saab &Aboeed, 2019).
ii)Rationale for medication: The drug acts fast and has a long-lasting effect on patients with breathing difficulties. The drug eases the bronchi and opens the airway for easier respiration and breathing in patients with airway constriction (Saab &Aboeed, 2019).
iii)Nursing considerations of medication: Several nursing considerations are associated with the administration of this medication. It must be noted that the administration of this drug in the patient can lead to buccal ulceration, dry mouth, headache, constipation, nausea, paradoxical bronchospasm, acute angle-closure glaucoma, immediate hypersensitivity, epistaxis, nasal dryness and paralytic ileus in adverse conditions(Beltaief et al., 2019). The hydration of the patient must be maintained to prevent incidences of hyperpyrexia (Saab &Aboeed, 2019).
iv)Expected clinical response: the patient response is expected to improve with better breathing due to clearing of the airways and bronchodilation this should result in restoration of the patient vitals including the normalization of the blood pressure, heart rate and oxygen saturation in the patient (Beltaief et al., 2019).
v) Continuing clinical observations required: The vitals of the patient must be essentially monitored to see improvements. The blood pressure, heart rate and oxygen saturation levels must be monitored regularly until normalized(Beltaiefet al., 2019).
References
Adlan, A. M., Veldhuijzen van Zanten, J. J., Lip, G. Y., Paton, J. F., Kitas, G. D., & Fisher, J. P. (2018). Acute hydrocortisone administration reduces cardiovagal baroreflex sensitivity and heart rate variability in young men. The Journal Of Physiology, 596(20), 4847-4861.
Barabutis, N., Khangoora, V., Marik, P. E., &Catravas, J. D. (2017). Hydrocortisone and ascorbic acid synergistically prevent and repair lipopolysaccharide-induced pulmonary endothelial barrier dysfunction. Chest, 152(5), 954-962.
Beltaief, K., Msolli, M. A., Zorgati, A., Sekma, A., Fakhfakh, M., Marzouk, M. B., ... &Belguith, A. (2019). Nebulized terbutaline and ipratropium bromide versus terbutaline alone in acute exacerbation of chronic obstructive pulmonary disease requiring noninvasive ventilation: a randomized double‐blind controlled trial. Academic Emergency Medicine, 26(4), 434-442.
Boulet, L. P. (2017). Pathophysiology of asthma. In Applied Respiratory Pathophysiology (pp. 67-96). USA: CRC Press.
Carpaij, O. A., Burgess, J. K., Kerstjens, H. A., Nawijn, M. C., & van den Berge, M. (2019). A review on the pathophysiology of asthma remission. Pharmacology & Therapeutics, 201, 8-24.
Saab, H., &Aboeed, A. (2019). Ipratropium. In StatPearls [Internet]. FL: StatPearls Publishing.
Sousa, M. P., & Warren, L. H. (2017). Acute management of respiratory distress in the adult patient. Simulation Scenarios for Nursing Educators: Making it Real, 11129.
Wilkinson, M., King, B., Iyer, S., Higginbotham, E., Wallace, A., Hovinga, C., & Allen, C. (2018). Comparison of a rapid albuterol pathway with a standard pathway for the treatment of children with a moderate to severe asthma exacerbation in the emergency department. Journal of Asthma, 55(3), 244-251.
Zhao, T., Liu, Z., Niu, J., Lv, B., Xiao, Y., & Li, Y. (2020). Investigation of the interaction mechanism between salbutamol and human serum albumin by multispectroscopic and molecular docking.BioMed Research International, 2020.
Zhou, L., Wang, Q., Zhang, Y., Ji, Y., & Yang, X. (2017). Aquatic photolysis of β2-agonist salbutamol: kinetics and mechanism studies. Environmental Science and Pollution Research, 24(6), 5544-5553.
Get It Done! Today
1,212,718Orders
4.9/5Rating
5,063Experts
Highlights
- 21 Step Quality Check
- 2000+ Ph.D Experts
- Live Expert Sessions
- Dedicated App
- Earn while you Learn with us
- Confidentiality Agreement
- Money Back Guarantee
- Customer Feedback
Just Pay for your Assignment
Turnitin Report
$10.00Proofreading and Editing
$9.00Per PageConsultation with Expert
$35.00Per HourLive Session 1-on-1
$40.00Per 30 min.Quality Check
$25.00Total
Free- Let's Start







