- Subject Code : NSG3RDP--NSG3RD
Case Analysis
Question 1
The condition of the patient, Joanna Cleese is deteriorating as evidenced by the vitals. The respiratory rate of the patient is 26 against the normal respiratory rate of 14-20 (McDonald &Eckhardt, 2017). The patient also has oxygen saturation at 94% that should ideally be above 96% (McDonald &Eckhardt, 2017). The GCS assessment of the patient reveals that she is confused and exhibits impairment in the analysis of time and place. The heart rate of the patient is 120 that is high against the normal heart rate of 60-100 bpm (Slater et al., 2016). The blood pressure of the patient is low with 90/55 mmHg (Slater et al., 2016). The vitals and signs assessed for Joanna indicate heart failure and the development of pulmonary edema. The critical cues that are associated with this include an abnormally increased respiratory rate of 26 breaths per minute in Joanna. The blood pressure of the patient has dropped and the respiratory rate has increased. Further, The ISBAR indicates ICC insitue 20cm suction, absence of swing, or bubbling 200mls frank blood drainage. The absence of swing indicates a blockage. The fluid in the chest drain tubing should rise with inspiration and fall with expiration. Failure to these observations the swings mark the presence of a blockage. Moreover, the lack of bubbling also indicates towards a blockage in Joanna. Patients with heart failure and pulmonary edema also have changes in the blood pressure (Freedman et al., 2016). The drop in blood pressure in heart failure is associated with the changes in the systolic and diastolic pressures. The reduced stroke volume in heart failure results in the dropping of the pulse pressure. Congestive heart failure is one of the most common causes of pulmonary edema. The primary factor that links pulmonary edema with heart failure is the failure of the left ventricle to function as an effective pump due to a discrepancy in the myocardial contractile strength and the load causing damage to the cardiac muscles impairing their function (Chanine&Alvey, 2019).
Since the organs in the body feel deprived of oxygen due to this reduced availability, the body tries to cope it with increased respiratory rate. Due to limited oxygen capacity, the oxygen saturation levels of the patient have also declined and a significant impact is observed on the cognitive abilities of the patient. In cases of heart failure, cognitive impairment is also observed (Freedman et al., 2016). As in the case of Joanna who presents signs of confusion regarding place and time, this occurs as the brain is not supplied adequate oxygen for its function causing confusion and dilemma in patients as experienced by Joanna.
Congestive heart failure occurs when the heart fails to meet the body's demands. In Joanna, a systolic heart failure is being observed. This condition occurs when the heart fails to pump blood appropriately to meet the metabolic demands of the body. Cardiogenic pulmonary edema us common dye to myogenic damage (Iqbal & Gupta, 2019). The systolic heart failure is also associated with hypertension and fluid overload. It is also evidenced by the 200mL leak in Joanna. Pulmonary edema is often caused in association with heart failure as in the case of Joanna. As the heart of the patient fails to pump blood efficiently throughout the body, the blood is backed up in the veins causing a hindrance in the blood transport (Iqbal & Gupta, 2019). The pressure in the blood vessels eventually increases and pushes the fluid in the alveoli, this restricts the normal oxygen availability in the lungs and consequently results in dyspnea (Chanine&Alvey, 2019). The health condition is presented by confusion and agitation also presented by Joanna. The hypotension of the blood pressure in this condition is associated with severe left ventricular systolic dysfunction in the patient. The left ventricular systolic dysfunction is associated with hypertension and increased cardiac workload. This results in the cardiomyopathy of the left ventricle. The hypertrophy of the muscle results in the loss of effective relaxation of the muscle. That impacts the cardiac output as it impairs cardiac filling. This impacts the ejection fraction and further impacts the pulmonary system and exacerbates the edema presenting the clinical symptoms in Joanna (Iqbal & Gupta, 2019).
Question 2
ABCDE assessment
The ABCDE assessment is an initial assessment and treatment with “Airway, breathing, circulation, disability, and exposure” (Steele et al., 2017). This assessment approach is used in all clinical emergencies for an immediate assessment and intervention application. This approach provides a systematic flow for the assessment and treatment of critical patients. ABCDE approach in the provided case study of Joanna helps to provide her with a life-saving treatment and break down complex clinical situations into the manageable condition. ABCDE approach also serves as an assessment and treating algorithm for clinicians and healthcare professionals. Further, it also manages to get minimal time to establish a final diagnosis and treatmentplans (Boyle &Bothamle, 2018). The approach applies to all patients irrespective of their age group. It is suggested that ABCDE assessment should be done when a critical illness or injury is suspected. Critical clinical situations like stroke and cardiac arrest present themselves with signs that can be assessed using the ABCDE approach and therefore can be prevented during the initial phases itself. As explained by the ABCDE approach, the airway problems are assessed first and treated, followed by assessment and treatment of breathing problems, followed by circulatory, disabling problems and exposure threats. It is suggested that after the initial ABCDE assessment, it should be repeated until the patient is stable (Steele et al., 2017). The assessment of airway through this approach includes assessing the voice and breath sounds, head tilt and chin lift with oxygen suction are recommended in case of anomalies. The breathing of the patient is assessed by checking the respiratory rate with chest wall movements and chest percussion, patient positioning and rescue breaths with inhaled medications are suggested. The circulatory problems of the critically ill patient are assessed by checking the skin color, capillary refill time, pulse rate and palpitation. The patients that express anomaly are provided IV access and infused saline with the management of bleeding if detected. In the next assessment, the disability of the patient is checked through the assessment of the level of consciousness (Taherkhani, 2018). The consciousness of the patient is inclusive of alertness, voice response, and pain response. Limbic movements and reflexes of the patient may also be assessed. The glucose levels of the patient are checked and are treated. For the assessment of exposure, body temperature and skin are assessed and treated for the underlying identified cause (Boyle &Bothamle, 2018).
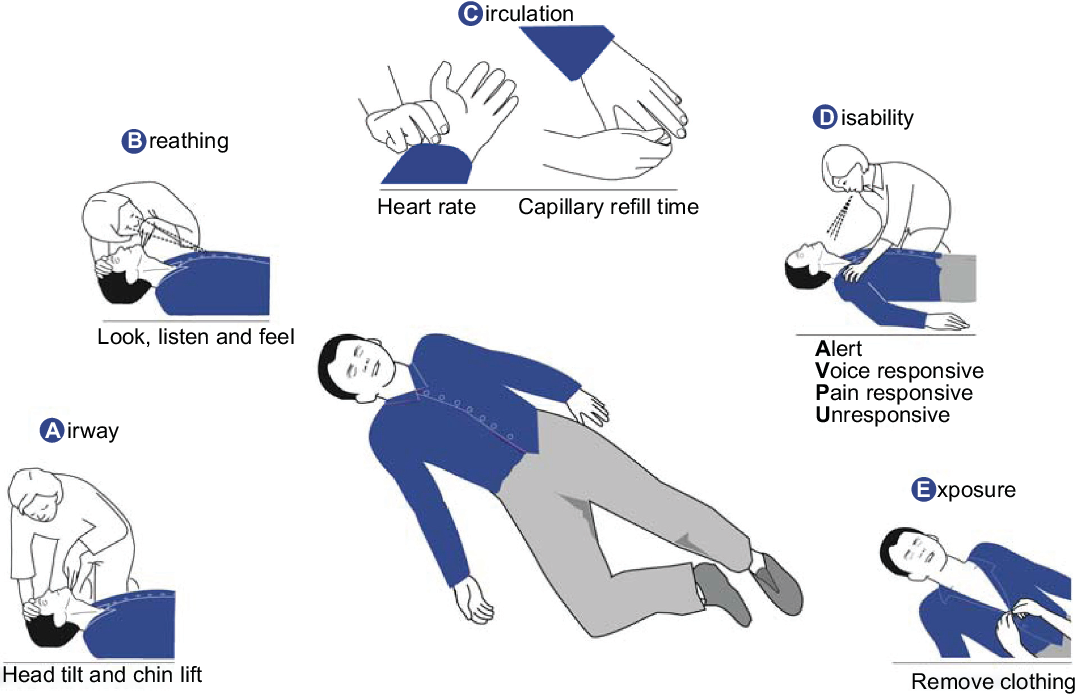
Figure 1: ABCDE assessment. (Source: Thim et al., 2012)
Head to toe assessment
The head to toe assessment is performed in a more general form whereas the ABCDE assessment is ideal for critical situations. The head to toe assessment provides a complete examination of the patient and is often initiated with the least invasive to the most invasive assessment to make the patient comfortable (Bryant, 2017). The head to toe assessment is done for the assessment and analysis of the overall health and general wellness of the patient. The head to toe assessment is inclusive of the level of alertness and cognition, state of health and the respiratory rate and therefore suitable for future assessments of Joanna. The assessment begins with an analysis of the general status of the patient. This is inclusive of an analysis of the vital signs, i.e. heart rate, temperature, blood pressure, oxygen saturation levels, pain, and pulse oximetry (McDonald &Eckhardt, 2017). Further, the assessment of the head, ears, nose, eyes, and throat is done. For this assessment, the lip color and moistness are observed, an inspection of teeth and gums is done. Buccal mucosa and palate are also assessed. The tongue, uvula, and tonsils are assessed followed by nose palpation and septal analysis. Hearing assessment of the patient is done and tympanic membrane and discharge are analyzed. Eye symmetry vision is also tested. Neck assessment in the patient involves checking of palpation in the lymph nodes, jugular venous distention and motion range of the shoulders is also analyzed. Cardiac assessment of the patient is also done by checking the temporal pulses and heartbeat (McDonald &Eckhardt, 2017). The abdomen of the patient is checked through the inspection of bowel sounds and tenderness. Further, in the head to toe assessment, pulses of the patient are also checked. The radial, posterior tibial, femoral and dorsalis pedis pulses are analyzed. Motion ranges, capillary refill, and sensation in the patient are also analyzed. The skin turgor of the patient is checked along with an assessment of the presence of any lesions or abrasions. Tensions, lumps, and tenderness in the skin are also critically observed. Further, the neurological assessment of the patient is also done by checking the orientation and assess the gait of the patient. Coordination and reflexes are also assessed and the Glasgow coma scale score is generated (Vincet et al., 2018).
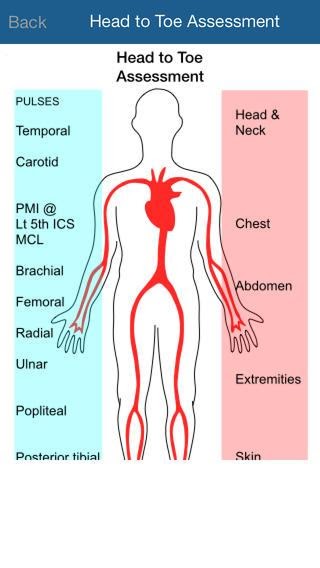
Figure 2: Head to toe assessment (Source: Bryant, 2017)
Question 3
Assessment of the respiration rate is considered crucial to determine the health and deteriorating condition of the patient. Respiratory rate is defined as several breaths taken by the patient per minute. This is a crucial vital sign and represents ventilation in the patient. A change in the respiratory rate is often considered as the first sign of clinical deterioration as the body of the patient struggles to maintain the oxygen availability to different tissues. It has been argued that early detection and assessment of changes in the vital signs, in particular, respiratory rate can help in the detection of respiratory failure. Respiratory compromise has been identified as one of the major causes of ICU admission from the general hospital wards (Vincet et al., 2018). In practice, the true assessment of the respiratory rate is also hindered as the patient may alter their breathing in awareness of the assessment. Another crucial lacuna that hinders adequate reporting of the respiratory rate is a lack of standard established. A generalized standard ranged adult respiratory rate between 12-16 breaths per minute (McDonald &Eckhardt, 2017). However, this is highly variable and can be altered based on the age of the patient, medication and other health conditions. Early detection of respiratory rate changes of about 3 breaths/ minute can be considered as early signs of deterioration (Dougherty & Lister, 2015). A higher respiratory rate than normal in the patients is indicative of anxiety, congestive heart failure, lung disease, drug overdose, and other complications. Whereas, lower than normal respiratory rate signals towards cardiac problems, drug overdose, and brain stem problems (Slater et al., 2016).
Effective measurement of respiratory rate is done by clinical monitoring of the number of breaths taken by the patient per minute through intervals of time. Various technologies like impedance pneumography are used for the assessment of respiratory rate. The electrical activity during inhalation and exhalation in assessed for accurate measurement. The limitation of this method is that the obstructions in the airflow may get undetected as chest wall movement records the respiration (Bradbrand et al., 2018). Capnography monitors are also an efficient tool to monitor the respiratory rate in the patients. The respiratory rate in the patients is measured by positioning the patient in a comfortable position in a relaxed state, ideally, the patient should be in rest for about 20 minutes before taking observations. The respiratory function of the patient should be tested with their ability to talk in complete sentences and alertness (Doughtery& Lister, 2015). The respiratory rate of the patient is often conjugated with oxygen saturation levels for a complete assessment (Bradbrand et al., 2018).
References
Boyle, M., &Bothamley, J. (2018). Critical care assessment by midwives. United Kingdom: Routledge.
Brabrand, M., Hallas, P., Folkestad, L., Lautrup-Larsen, C. H., &Brodersen, J. B. (2018). Measurement of respiratory rate by multiple raters in a clinical setting is unreliable: A cross-sectional simulation study. Journal of Critical Care, 44, 404-406.
Bryant, S. G. (2017). Keeping it in the program: Second year nursing students as stand-in patients for first year head-to-toe assessment check-offs. Nurse Educator, 42(2), 60-61.
Chahine, J., &Alvey, H. (2019). Left Ventricular Failure. In StatPearls [Internet]. StatPearls Publishing.
Dougherty, L. &Lister, S. (2015) The royal Marsden manual of clinical nursing procedures. USA: Oxford: Wiley-Blackwell.
Freedman, B., Potpara, T. S., & Lip, G. Y. (2016). Stroke prevention in atrial fibrillation. The Lancet, 388(10046), 806-817.
Iqbal, M. A., & Gupta, M. (2019). Cardiogenic Pulmonary Edema. In StatPearls [Internet]. StatPearls Publishing.
Johnson, V., Schmitt, J., & Hamm, C. W. (2017). Stroke prevention in atrial fibrillation–latest guideline recommendations and real world data. MedizinischeMonatsschrift fur Pharmazeuten, 40(4), 167-170.
Kamel, H., Okin, P. M., Elkind, M. S., &Iadecola, C. (2016). Atrial fibrillation and mechanisms of stroke: Time for a new model. Stroke, 47(3), 895-900.
McDonald, K., & Eckhardt, A. L. (2017). Evidence-based practice in action: ensuring quality of pediatric assessment frequency. Journal of Pediatric Nursing, 35, 134-138.
Slater, L. Z., Bryant, K. D., & Ng, V. (2016). Nursing student perceptions of standardized patient use in health assessment. Clinical Simulation in Nursing, 12(9), 368-376.
Steele, A., Greenwood, M., & Desai, H. (2017). ABCDE assessment and the out-of-hospital cardiac arrest. Dental Update, 44(10), 1003-1009.
Taherkhani, A. (2018). Use of the ABCDE approach to assess a patient post-operatively: A case study. Nursing Standard.10, 55.
Thim, T., Krarup, N. H., Grove, E. L., Rohde, C. V., &Løfgren, B. (2012). Initial assessment and treatment with the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach. International Journal of General Medicine, 5, 117–121.
Vincent, J. L., Einav, S., Pearse, R., Jaber, S., Kranke, P., Overdyk, F. J., Whitaker, D. K., Gordo, F., Dahan, A., &Hoeft, A. (2018). Improving detection of patient deterioration in the general hospital ward environment. European Journal of Anaesthesiology, 35(5), 325–333.
Get It Done! Today
1,212,718Orders
4.9/5Rating
5,063Experts
Highlights
- 21 Step Quality Check
- 2000+ Ph.D Experts
- Live Expert Sessions
- Dedicated App
- Earn while you Learn with us
- Confidentiality Agreement
- Money Back Guarantee
- Customer Feedback
Just Pay for your Assignment
Turnitin Report
$10.00Proofreading and Editing
$9.00Per PageConsultation with Expert
$35.00Per HourLive Session 1-on-1
$40.00Per 30 min.Quality Check
$25.00Total
Free- Let's Start







